Введение
Мочевая кислота (МК), как известно, является конечным продуктом распада пуриновых оснований в процессе метаболизма нуклеиновых кислот. Элиминация МК осуществляется через почки, однако в силу определенных причин ее концентрация в тканях увеличивается. На этот процесс влияет и усиленное образование МК, и нарушение элиминации. Наиболее известной причиной повышения уровня МК считается повышенное потребление фруктозы и/или мясных продуктов [1] либо острое или хроническое почечное повреждение.
Более того, соли МК сами по себе способны приводить к хроническому поражению почек, что также сопровождается прогрессивным накоплением МК и ее солей [2]. Как следствие повышения уровня МК развивается метаболический синдром, т.е. повышение уровня артериального давления, сахара крови, триглицеридов и массы тела [3–7]. Хорошо известные кожные проявления гиперурикемии (зуд, эритема, гиперчувствительность) также представляют серьезную диагностическую проблему на ранних этапах развития заболевания. В свою очередь тофусы, развивающиеся при длительной гиперурикемии, представляют серьезную проблему в плане терапии. Причем опасность представляют концентрации МК от 300 мкг/л, т.е. значения, принятые как нормальные. Отмечена также связь между уровнем МК и развитием системного атеросклероза [5], сахарного диабета 2 типа [8, 9], жирового гепатоза [10].
С целью снижения МК кроме коррекции диеты при подагре обычно используются препараты типа аллопуринола, препятствующие образованию МК [11–14]. Однако данные препараты обладают выраженными побочными эффектами, в частности гепатотоксичностью. Кроме того, при длительном употреблении снижается их эффективность. Следует иметь в виду, что аллопуринол или бензмарон практически не влияет на уже депонированные в тканях соли МК.
Вместе с тем известно, что ряд растительных экстрактов при регулярном использовании оказывает лечебное действие при подагре. В традиционной и официальной медицине есть упоминание об эффективности экстрактов таких растений, как осина, береза, таволга, при подагре [15, 16]. Кроме того, показано, что комплекс активных компонентов, таких как флавоноиды и органические кислоты, способны снижать продукцию и/или усиливать экскрецию МК [17, 18]. В частности, флавоноиды кверцитин и байкалин служат эффективными блокаторами ксантиноксидазы, ключевого энзима в продукции МК [19, 20].
Достоинством растительных компонентов является минимальное количество побочных эффектов и возможность длительного использования в качестве дополнения к основной либо лечебной диете, либо в виде самостоятельного растительного лекарственного препарата.
Цель исследования: оценка эффективности биологически активной добавки (БАД) на основе растительных компонентов таволги вязолистной (Filipéndula ulmária) и осины (Pópulus trémula) в снижении уровня МК у пациентов с исходно повышенным ее уровнем, а также оценка кожных изменений при подагре.
Методы
Исследование носило пилотный характер, проведено в соответствии с рекомендациями по проведению клинических исследований. В исследовании принимали участие пациенты с повышенным уровнем МК сыворотки крови (более 350 мкмоль/л у женщин и 415 мкмоль/л у мужчин). В исследовании приняли участие 109 пациентов в возрасте 45–65 лет, из них 47 мужчин (группа 1) и 62 женщины (группа 2). На время исследования пациенты сохраняли рекомендованную диету и питьевой режим. Такие проявления, как зуд, эритема и/или гиперчувствительность кожных покровов, отмечены у 45 пациентов, т.е. в 42% случаев. Тофусы имели место у 12 пациентов (11% от общего числа пациентов).
Исследовалась активность микронизированных (до размеров частиц 0,01–0,001 мм) стеблей таволги и коры осины в соотношении 1:1 в составе исследуемой БАД (Патент РФ RU 2683570). Прием препарата осуществлялся в капсулированном виде в дозе 0,5 г/сут в течение 30 дней.
Уровень МК определяли до применения композиции, по окончании курса и через месяц после окончания курса. Кроме того, определяли уровень сахара крови и триглицеридов до начала и сразу после окончания приема препарата.
Статистическая обработка проводилась с использованием пакета Статистика 10.0, результаты были представлены как М±m, уровень достоверности принимался при p<0,05.
Результаты
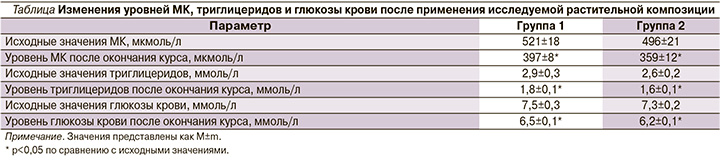
Оценивались эффективность композиции исследуемой БАД, продолжительность гипоурикемического действия, а также влияние на углеводный обмен и концентрацию триглицеридов сыворотки крови. Результаты представлены в таблице.
У большинства пациентов с исходной гиперурикемией отмечено повышенное содержание триглицеридов (более 1,7 ммоль/л, всего 76% пациентов 1-й группы и 68% второй), а также сахара крови (более 6,0 ммоль/л, 80% в 1-й группе и 74% во второй).
После использования исследуемой композиции у всех пациентов отмечено снижение МК. В целом уровень МК в группе 1 снизился на 24% (p<0,05) и на 27% во второй (p<0,05; см. таблицу). При исследовании МК через месяц после окончания приема композиции достоверных изменений уровня МК не отмечено как в 1-й (403±8 мкмоль/л), так и во 2-й группах (345±10 мкмоль/л). Только у двух пациентов 1-й группы уровень МК, будучи сниженным, вновь незначительно превысил нормальные значения. Таким образом, достигнутый эффект сохранялся и спустя месяц после прекращения приема препарата.
У пациентов с исходно повышенным уровнем триглицеридов отмечено их достоверное снижение с 2,9±0,3 до 1,8±0,1 ммоль/л (р<0,05) в первой группе и с 2,6±0,2 до 1,6±0,1 ммол/л во второй (р<0,05). Достоверное снижение уровня сахара крови также отмечено у пациентов обеих групп (на 13 и 15% соответственно, различия достоверны). Тенденция к нормализации уровней триглицеридов и сахара крови пациентов с исходной гиперурикемией также свидетельствует о реальной коррекции пуринового обмена и уровня МК вследствие действия исследуемой композиции.
Через месяц после начала приема препарата 89% пациентов указали на исчезновение таких проявлений, как зуд и эритема, и 50% указали на положительные изменения со стороны подкожных образований (тофусов).
В частности, исчезали свищи и серозное отделяемое из подкожных образований, а также происходило существенное уменьшение их размеров.
В качестве побочного эффекта у 5% пациентов группы 1 и 3% пациентов группы 2 испытывали кратковременные болезненные ощущения в области проекции печени и желудка, не требовававшие медикаментозной коррекции. У одного пациента использование препарата было прекращено вследствие аллергической реакции (аллергический ринит). Токсических эффектов, а также тошноты или рвоты не отмечено.
Обсуждение
Исследованная БАД на основе растительных компонентов таволги и осины показала безопасность и высокую эффективность в снижении уровня МК в сыворотке крови. Данный эффект сохранялся после прекращения приема препарата. Кроме того, отмечена высокая эффективность в снижении уровней триглицеридов и сахара крови пациентов с исходно повышенными их концентрациями.
Изменения со стороны уровня МК сочетались с исчезновением или значительным улучшением со стороны кожных проявлений.
Предполагаемый механизм действия препарата связан как со снижением продукции МК за счет снижения активности ксантиноксидазы, так и с усилением клиренса МК и ее солей из сыворотки крови и других тканей [15, 16].
Заключение
Исследованная БАД на основе растительных компонентов таволги вязолистной (Filipéndula ulmária) и осины (Pópulus trémula) может быть рекомендована к использованию при повышенном уровне МК и подагре как компонент функционального питания или самостоятельный растительный препарат. Эффективно устраняет кожные проявления выраженной гиперурекемии, такие как зуд, гиперемия, гиперчувствительность.



