Введение
Интерстициальные заболевания легких (ИЗЛ) у детей представляют собой многообразие нозологических форм, характеризующихся поражением альвеолярных структур и периальвеолярной интерстиции [1]. В настоящее время ряд острых заболеваний протекает с интерстициальными изменениями в легочной ткани и клинической картиной ИЗЛ, однако характеризуются благоприятным прогнозом и отсутствием трансформации в хроническое заболевание. К подобным формам относят острые бронхиолиты (ОБ) у детей. Актуальность изучения бронхиолитов обусловлена их высокой частотой у детей первого года жизни, нередко тяжелым течением, требующим стационарного лечения и интенсивной терапии. Так, согласно современным представлениям, бронхиолит наиболее часто встречается у детей в возрасте до 9 месяцев (90% случаев). Ежегодно в мире регистрируется 150 млн случаев бронхиолита (11 заболевших на 100 детей грудного возраста), 7–13% из которых требуют стационарного лечения, и 1–3% – госпитализации в отделение интенсивной терапии [1, 2]. Сезонный пик заболеваемости бронхиолитом в наших географических широтах продолжается с ноября по апрель. К основным возбудителям заболевания относят респираторно-синцитиальную (РС; Human Respiratory Syncytial virus) вирусную инфекцию (60–70%). У недоношенных, особенно у детей с бронхолегочной дисплазией (БЛД) и находящихся на искусственном вскармливании, этиологически значимым агентом при бронхиолите может быть риновирус (до 40% случаев). Как причинные факторы заболевания также рассматриваются вирусы гриппа А и В, парагриппа, адено-, корона-, метапневмо- и бокавирусы человека [1].
Как известно, клиническая классификация бронхиолитов основана на этиологии, при этом помимо инфекционных агентов рассматриваются системные заболевания, при которых бронхиолит развивается как один из синдромов. С учетом пандемии коронавирусной инфекции, в результате которой наблюдалось изменение реактивности бронхолегочной системы, инверсии течения многих бронхолегочных заболеваний с развитием ранее не диагностированных состояний нами проведен клинический анализ течения бронхиолитов у детей Астраханской области.
Цель исследования: изучить вариабельность клинической картины, данных лабораторно-инструментальных методов исследования, методов медикаментозной терапии детей с различными формами бронхиолитов.
Методы
Проведено клиническое наблюдение за детьми с различными формами бронхиолитов в Астраханской области, получавших лечение на базе пульмонологического отделения ГБУЗ АО «ОДКБ им. Н.Н. Силищевой» в период с 01.2022 по 30.04.2023.
Различные формы бронхиолитов за данный период диагностированы у 13 пациентов: острые формы у 11 больных, хронический облитерирующий у 1 (возраст – 8 лет 7 месяцев), интерстициальная болезнь легких в форме фолликулярного бронхиолита рассматривалась как компонент первичного иммунодефицита (синдрома Луи-Бара) у 1 пациента (возраст 4 года 3 месяца).
Количество мальчиков превышало число девочек и составило 9 и 4 соответственно.
Из 11 детей с ОБ семеро были в возрасте от 4 месяцев до 2 лет (средний возраст – 1,3 ±0,38 года ) и 4 детей от 10 до 15 лет ( средний возраст – 11±1,94 года). Дети младшей возрастной группы первоначально проходили обследование и лечение в инфекционном стационаре города, однако в связи с сохраняющейся клинической картиной после купирования лихорадки и катаральных явлений были переведены в пульмонологическое отделение ГБУЗ АО «ОДКБ им. Н.Н. Силищевой» Астрахани.
Исследование проводилось на основе собственных наблюдений и данных медицинской документации. У всех пациентов оценивались личный и семейный анамнез, выраженность основных клинических проявлений, (тахипноэ, степень дыхательной недостаточности, вариабельность аускультативной картины в легких), а также ответ на проводимую терапию.
Все наблюдаемые дети обследованы общепринятыми клинико-лабораторными методами, включая общеклинические анализы, биохимические исследования крови. Согласно клиническим рекомендациям, для уточнения этиологического фактора проводились дополнительные иммунологические и вирусологические исследования в условиях инфекционного стационара. Вирусологическое обследование включило определение респираторно-синцитиального вируса, рино-, бока-, вируса гриппа А и В, адено- (в условиях инфекционного стационара), коронавирусов.
Рентгенологические методы обследования включили рентгенограмму органов грудной клетки и/или компьютерную томографию высокого разрешения для детального изучения характера изменений в легочной ткани.
Определение показателей функции внешнего дыхания с учетом возраста обследованных пациентов проводилось двумя способами: детям младшего возраста (до 6 лет) с помощью бронхофонографии, пациентам по достижении 6 лет, когда становится возможным выполнение адекватных дыхательных паттернов – спирометрии.
Результаты
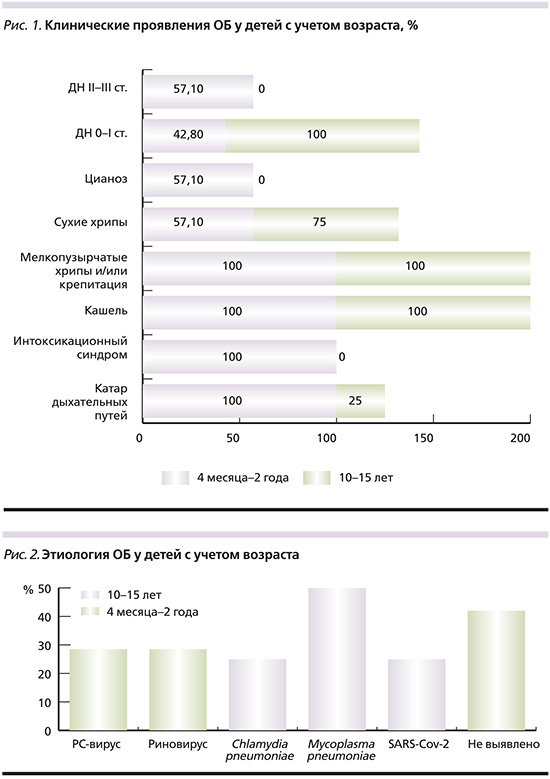
Клиническая картина острых бронхиолитов характеризовалась непродуктивным кашлем, проявлениями дыхательной недостаточности, крепитацией и мелкопузырчатыми хрипами в легких при аускультации. В ходе наблюдения определены различия в клинической картине у детей разных возрастных групп. У детей младшего возраста (n=7; средний возраст – 1,3±0,38), согласно данным анамнеза, заболевание стартовало с фебрильной или субфебрильной лихорадки, катара верхних дыхательных путей, интоксикационного синдрома с последующим (в течении 2–6 дней) развитием дыхательной недостаточности, которая носила среднетяжелый и тяжелой характер, что потребовало в ходе госпитализации перевода в реанимационное отделение 4 из 7 детей Длительность различных вариантов вентиляционной поддержки в данной группе варьировалась от 1 до 4 недель. В старшей возрастной группе (n=4; средний возраст – 11±1,94) развития интоксикационного синдрома отмечено не было, а степень дыхательной недостаточности не превышала первую (рис. 1).
Течение облитерирующего бронхиолита у наблюдаемой нами больной носило благоприятный характер: несмотря на длительный стаж заболевания (8 лет), обострения бронхолегочного процесса были средней тяжести, единичными и ассоциировались с острыми респираторными вирусными инфекциями; прогрессирования дыхательной недостаточности не наблюдалось, сохранялись нормальные темпы роста и физического развития.
В период ремиссии отсутствовали одышка и постоянный кашель, однако выслушивались влажные мелкопузырчатые хрипы и крепитация в нижних отделах левого легкого, прослеживалась деформация ногтевых пластин по типу «часовые стекла».
При проведении лабораторной диагностики у детей с инфекционными формами бронхиолитов в общеклинических анализах крови изменений не выявлено. Положительный результат теста полимеразной цепной реакции (ПЦР) на РС-вирус (2 пациента) и риновирус (2 пациента) подтвердил этиологическую роль в развитии заболевания у пациентов младшего возраста.
У 2 пациентов старшего (10 и 16 лет) возраста выявлены IgM к Mycoplasma pneumoniae, у 1 – IgM к Chlamydia pneumoniae, что позволило расценивать данные возбудители в контексте особенностей клинической картины как этиотропные. У ребенка с перенесенной коронавирусной инфекцией в дебюте заболевания отмечен положительный результат ПЦР-теста (мазок из носоглотки) на COVID-19, а в дальнейшем – нарастание титра IgG к SARS-CoV-2.
При оценке функции внешнего дыхания у детей старшей возрастной группы определен обструктивно-рестриктивный (у 3 больных) или рестриктивный тип нарушений (у 1 пациента). В младшем возрасте у всех пациентов определено выраженное нарушение проходимости на уровне средних и нижних дыхательных путей, о чем свидетельствовала фиксация средне- и высокочастотных частотных шумов при проведении исследования.
По данным компьютерной томограммы наблюдались типичные проявления острого бронхиолита в виде участков «матовое стекло», зон мозаичной олигемии с центролобулярными узелками (признак «дерево в почках»), при этом у детей с диагностированной бронхолегочной дисплазией отмечены характерные изменения в виде фиброзных тяжей в дорзальных отделах (рис. 3, 4).

Лечение детей младшего возраста с острым бронхиолитом включило адекватную гидратацию, респираторную поддержку, ингаляционную терапию гипертоническим раствором NaCl 3% в отсутствие противопоказаний [3]. С учетом диагностированного бронхообструткивного синдрома, тяжести состояния, коморбидной патологии у 4 пациентов младшего возраста (57,1%) в комплекс лечения включены системные и ингаляционные формы глюкортикостероидов. Трое детей в условиях реанимационного отделения получали антибактериальные препараты.
В комплекс лечения больных старшей возрастной группы с идентифицированной атипичной флорой включены препараты из группы 14- и 16-членных макролидов. На фоне терапии острых инфекционных бронхиолитов отмечено клинико-рентгенологическое разрешение заболевания у 100% пациентов.
Длительность госпитализации детей с ОБ варьировалась от 7,2 ±2,4 суток у детей старшей возрастной группы и до 14,3 ± 4,2 у детей первых 2 лет жизни.
Интерстициальная лимфоцитарная болезнь легких в виде фолликулярного бронхиолита диагностирована у одного ребенка с первичным иммунодефицитом – атаксией–телеангиэктазией (синдромом Луи-Бара). При развитии клинических проявлений у пациента доминировала бронхолегочная симптоматика в виде сухого малопродуктивного кашля, нарастающей дыхательной недостаточности постоянно, отставания в физическом развитии. Аускультативно отмечены постоянные крепитация и мелкопузырчатые хрипы с тенденцией к увеличению при обострении бронхолегочного процесса, спровоцированного вирусными инфекциями. За время исследования прослежено нарастание жалоб неврологического характера (пошатывание при ходьбе, неловкая походка, нарушение тонкой моторики, задержка в речевом развитии, эмоциональная неустойчивость) при полном отсутствии кожных проявлений в виде телеангиоэктазий и витилиго. Для комплексной оценки функции легких «золотым» стандартом остается спирометрия, однако данное исследование не проводилось ввиду возрастных ограничений и проявления миопатии. По данным КТ органов грудной клетки определялись характерные участки «матовое стекло», неравномерность пневматизации (рис. 5).
Компьютерная томограмма проводилась не чаще 1 раза в год с учетом высокого риска развития онкологической патологии у данного пациента. Несмотря на достаточно четко описанные рентгенологические характеристики ИЛБЛ, достоверным критерием является гистологическая верификация диагноза. Посредством торакоскопической биопсии легкого получен гистологичекий материал. Морфологическая картина представлена гиперплазированными лимфоидными фолликулами, расположенными вокруг бронхиол c частичной и полной облитерацией бронхиальной пластинки, но с минимальной заинтересованностью альвеолярной мембраны. Современные стратегии ведения пациента основаны на междисциплинарном лечении проявлений болезни. С момента постановки диагноза и по настоящее время ребенку проводится заместительная терапия внутривенными иммуноглобулинами 1 раз в 4 недели в сочетании с препаратом таргетной терапии Абатацептом. Несмотря на проводимое лечение, наблюдаются нарастание тяжести дыхательной недостаточности, частые обострения бронхолегочного процесса по пневмоническому типу с выраженным регрессом функциональных показателей и изменений по данным имидж-диагностики.
Обсуждение
Тяжелое течение заболевания отмечено преимущественно у детей до 2 лет. По нашему мнению, тяжесть респираторной симптоматики у детей младшего возраста связана как с возрастными анатомо-физиологическими особенностями строения дыхательной системы, так и с отягощенным коморбидным фоном (диагностированной ранее бронхолегочной дисплазией тяжелой степени [у 3 пациентов] и неконтролируемой формой эпилепсии (у 1 ребенка) У детей старшей возрастной группы дыхательная недостаточность не превышала 1-ю степень, а в спектре возбудителей превалировали представители бактериальной атипичной флоры, такие как Mycoplasma pneumoniae и Chlamydophila (Chlamidia) pneumoniae. Мы не исключаем, что интерстициальные изменения в легких данной категории больных были ассоциированы с ранее перенесенной коронавирусной инфекцией. Согласно исследованиям, проведенным российскими учеными, у детей и подростков, перенесших коронавирусную инфекцию, может наблюдаться как девиация клинической картины и течения респираторных инфекций, так и длительно сохраняющиеся в легких изменения в виде «матового стекла» при проведении компьютерной томографии высокого разрешения [4, 5]. Однако расширенный спектр вирусологической диагностики не был нам доступен с учетом терапевтического профиля стационара, а не инфекционного, что не позволило сделать окончательные выводы. Информационный поиск о причинах острого бронхиолита в подростковом возрасте был не результативен. В то же время, согласно данным отечественной литературы, реализация заболевания у взрослых рассматривается как результат длительного курения, иммунопатологических состояний, постинфекционного генеза с реализацией облитерирующего процесса и криптогенной этиологии [6], при этом среди инфекционных факторов рассматриваются и такие возбудители, как Mycoplasma pneumoniae и Chlamydophila pneumoniae. У детей раннего возраста острый бронхиолит чаще развивается в ответ на респираторно-синцитиальную вирусную (РСВ) инфекцию (20–75%) и риновирус (до 40% случаев), на долю иных вирусов (парагриппа, адено-, корона-, метапневмо- и бокавируса) приходится не более 5–1 % [1, 2]. Результаты нашего исследования согласуются с ранее проведенными и описанными в литературе.
Согласно нашему исследованию, у детей младшего возраста с тяжелым течением ОБ в условиях реанимационного отделения в комплекс лечения включены антибактериальные препараты. Однако назначение данной группы обоснованна при объективизации бактериальной инфекции. Так, согласно мета-анализу 2021 г., присоединение бактериальных осложнений при остром бронхиолите составляет не более 1% [7, 8]. В ряде проведенных исследований не отмечено положительной динамики, а также уменьшения сроков госпитализации на фоне рутинного использования антибактериальной терапии при ОБ, за исключением тех случаев, где имеется присоединение вторичной бактериальной инфекции [9–13]. Таким образом назначение а/б препаратов должно носить исключительно персонифицированный характер, исходя из динамики клинической картины, лабораторных маркеров бактериальной инфекции, анализа коморбидных и мультиморбидных состояний каждого конкретного пациента. Назначение ингаляционных и системных глюкокортикостероидов при тяжелом течении бронхиолита считается обоснованным при наличии синдрома бронхиальной обструкции, тяжелого течения бронхолегочной дисплазии. Наличие отягощенного коморбидного фона не снижает продолжительности стационарного лечения (по сравнению с группой плацебо разница в сроке госпитализации составила -0,18 дня) [14].
В нашем исследовании у одного ребенка отмечено развитие ИЗЛ в виде лимфоцитарной болезни легких на фоне первичного иммунодефицита (синдром Луи-Бара), при этом клинические проявления поражения легких стартовали ранее других симптомов данного синдрома и являлись основными, обусловливающими тяжесть течения заболевания. Несмотря на орфанность и гетерогенность ПИД, поражения легких, согласно проведенным исследованиям, встречается более чем в 40% случаев и может быть представлена как рецидивирующими бактериальными инфекциями, так и лимфоцитарной болезнью легких, включившей фолликулярный бронхиолит, лимфоцитарную интерстициальную пневмонию, нодулярную лимфоидную гиперплазию [15].
Исход бронхиолита во многом зависит от его формы. Согласно литературным данным, прогноз после перенесенного ОБ, как правило, благоприятный. Респираторные симптомы средней степени выраженности могут сохраняться приблизительно 3 недели, однако около половины пациентов, перенесших острый бронхиолит, в дальнейшем могут иметь эпизоды бронхиальной обструкции, при этом уделяется особое внимание пациентам с отягощенной наследственностью по атопии, для которых бронхиолит может быть одним из факторов риска развития бронхиальной астмы [1, 9]. Иным исходом острого бронхиолита может быть формирование постинфекционного облитерирующего бронхио-лита, характеризующегося хроническим течением с развитием фиброза и облитерацией просвета бронхиол, инвалидизацией. Наши данные совпадают с литературными, все дети с острым бронхиолитом выписаны с улучшением под наблюдение педиатра с дальнейшим полным разрешением воспалительного процесса в легких.
Заключение
На сегодняшний день бронхиолиты у детей сохраняют свою актуальность, трансформировались из заболевания детей младшего возраста в пульмонологическую проблему всего педиатрического возраста, гетерогенные по характеру клинической картины и этиопатогенетическим факторам, что требует проведения диагностического поиска и персонифицированного подхода к терапии при ведении пациентов с данной нозологической формой.
Вклад авторов. Концепция и дизайн исследования – Д.Ф. Сергиенко. Сбор и обработка материала – Д.Ф. Сергиенко. Статистическая обработка данных – Д.Ф. Сергиенко. Написание текста – Д.Ф. Сергиенко. Редактирование – О.А. Башкина.