Актуальность
Проблема туберкулеза (ТБ) актуальна и в условиях снижения заболеваемости и смертности – отчасти из-за сложностей его полноценного клинического излечения [1]. По истечении года химиотерапии удается добиться стойкого прекращения бактериовыделения и закрытия полостей распада у 70–60% впервые выявленных пациентов [2], если же отдельно рассматривать эффективность лечения ТБ при наличии множественной лекарственной устойчивости возбудителя, то она еще ниже при условии более длительного курса химиотерапии [1, 3, 4].
Хроническая обструктивная болезнь легких (ХОБЛ) относится к числу широко распространенных хронических неинфекционных заболеваний, заболеваемость и смертность от которой, к сожалению, продолжают расти. В эпидемиологически неблагоприятных регионах с высоким уровнем заболеваемости ТБ высока вероятность сочетания этих заболеваний. В связи с чем вопросы присоединения, его развития и течения у коморбидных пациентов на сегодняшний день изучены недостаточно и требуют дальнейшей разработки [5–7].
В литературе имеются отдельные публикации, направленные на поиск факторов, определяющих риск развития ТБ, но основная их часть касается социальных или эпидемиологических аспектов [8–10], в связи с чем актуально выделение медицинских параметров, которые могут влиять на исход лечения ТБ.
Было решено проанализировать степень влияния отдельных медицинских параметров на возможность присоединения ТБ и последующие исходы его лечения у пациентов с коморбидной патологией.
Цель исследования: выделение корригируемых медицинских факторов, повышающих риск неблагоприятного исход лечения ТБ у пациентов с ТБ и ХОБЛ, для разработки мероприятий по повышению эффективности лечения.
Методы
Исследование простое одномоментное. В него включены 204 пациента, поступивших в БУЗОО «Клинический противотуберкулезный диспансер № 4» (КПТД № 4) и БУЗОО «Клинический противотуберкулезнй диспансер» (КПТД) в течение года с диагнозом впервые выявленного ТБ и ХОБЛ. Из них было 180 мужчин (88,2%) и 24 женщины (11,8%; χ2=41,15, p=0,000) в возрасте (Ме (25,0; 75,0) 48,25 года (38,00; 57,00) (см. таблицу). Критерии включения: наличие впервые ТБ, наличие ХОБЛ, согласие пациента на участие в исследовании.

Критерии исключения: внелегочный ТБ, злокачественные новообразования.
Диагноз ТБ выставлялся на основании клинико-рентгенологических данных, был подтвержден результатами бактериологического исследования [8, 11] 172 (84,3±2,5%) пациенов методами микроскопии, 166 (81,4±2,7%) пациентов– молекулярно-генетическими методами (МГМ), результатами кожных иммунологических тестов [1, 12, 13] – Диаскин-тест положительный – 193 (94,6±1,6%) пациентов (см. таблицу).
Диагноз ХОБЛ был выставлен на основании клинико-анамнестических данных и инструментальных методов исследования (спирометрии). Курящими были 198 (97,1±1,2%) пациентов (анамнез курения Ме (25; 75) 27,5 (20; 40) пачка/лет), 12 (5,9±1,6%) пациентов имели производственные вредности (см. таблицу).
Исход ТБ у пациентов с ХОБЛ может быть обусловлен действием множества разнообразных причин, а результаты измерений совокупности этих признаков представляют в виде многомерных случайных величин. В качестве математического аппарата для выявления интегративных латентных характеристик как факторов риска предлагается использовать методы факторного анализа (ФА). Они позволяют формировать и выявлять значимые факторы. Основой любого метода ФА служит обработка линейных корреляционных связей между измеряемыми показателями, поэтому на первом этапе формируется корреляционная матрица с одновременной проверкой на нормальность распределения. Далее осуществляется выбор метода ФА, с помощью которого находится матрица корреляции между искомыми факторами и исходными показателями матрица весовых нагрузок [14, 15].
В данной исследовательской работе использован метод главных факторов с варимаксвращением, а для определения количества факторов – метод Гуттмана с эффектом «каменистой осыпи» [15]. Расчет матрицы весовых нагрузок осуществляется не для всех таблиц исходных данных, а только для тех, которые исследователь рассматривает как основу выявления факторов риска [14, 15].
Результаты исследования
Величины собственных значений и веса факторов показывают, что механизм формирования исходов ТБ у коморбидных пациентов многокомпонентен.
Для анализа взяты 47 медицинских параметров, полученных в результате инструментального обследования включенных в исследование больных, пациентам было проведено суточное мониторирование артериального давления (СМАД), эхокардиография (ЭхоКГ), спирография (СПГ). Оценивалось влияние состояния центральной гемодинамики (по показателям СМАД), изменения структуры и функций сердечной мышцы (по параметрам ЭхоКГ), функциональной активности легких (по показателям СПГ), характеристик туберкулезного процесса на исход туберкулеза у коморбидных (ТБ+ХОБЛ) пациентов (рис. 1).
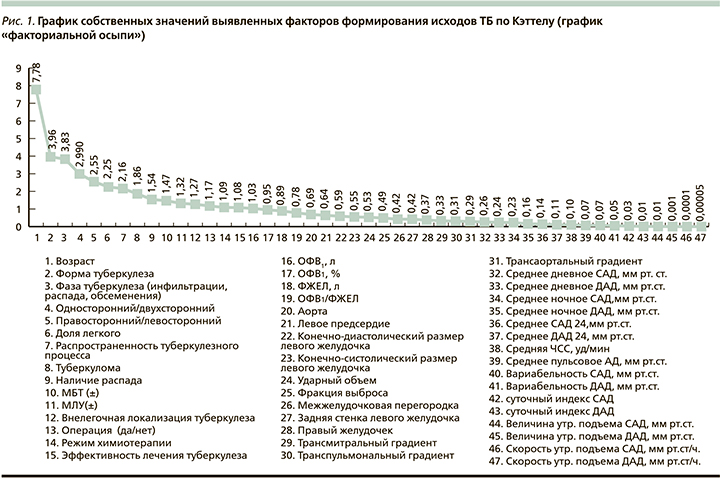
Дисперсия, объясненная 17 последовательными факторами, составляла 81,3% вклада всех факторов, что свидетельствует о достаточной адекватности разработанной модели (рис. 2).

Первый (I) из них можно условно определить как «сосудистый фактор», или фактор «центральная гемодинамика: эффективность кровотока», его вклад в прогноз при туберкулезе у коморбидных пациентов составил 16,09%, и он распределился между несколькими параметрами, связанными между собой: среднедневное систолическое артериальное давление (САД); среднедневное диастолическое артериальное давление (ДАД); средненочное САД; средненочное ДАД; среднее САД; среднее ДАД; среднее пульсовое АД; вариабельность САД. Нестабильность гемодинамических данных, проявляющаяся неконтролируемым АД, входит в число факторов, которые в совокупности будут влиять на соматическое состояние и увеличивать риск ТБ.
Второй (II) фактор, от которого зависит прогноз при ТБ у коморбидных больных, определен как «распространенность туберкулезного процесса», его вклад составил 7,35%. Он включает следующие параметры: двусторонний процесс; многодолевое поражение. Эти параметры, как показано результатами ФА, уступают сосудистому фактору, если это касается коморбидных пациентов.
Третий (III) фактор с вкладом в прогноз 6,16% определен как «систолическая функция сердца» (насосная функция сердца), включает три параметра: конечно-диастолический размер левого желудочка; конечно-систолический размер левого желудочка; ударный объем левого желудочка левого. Составляющие данного фактора определяют состояние насосной функции сердца, что важно учитывать коморбидным пациентам.
Снижение насосной функции сердца влечет за собой снижение ударного объема, что опять же нарушает нормальное функционирование сердечно-сосудистой системы и делает пациентов уязвимыми в плане полноценного излечения туберкулезного процессов.
Четвертый (IV) фактор с вкладом в прогноз при ТБ у коморбидных больных 5,45% определен как «ремоделирование сердца», включает два параметра, определяемых по ЭхоКГ, таких как изменение размера межжелудочковой перегородки и размер задней стенки левого желудочка.
Этот фактор характеризует компенсаторные возможности сердечной мышцы при работе в условиях повышенных нагрузок, у коморбидных пациентов при присоединении ТБ наблюдается увеличение нагрузки на сердце, и в отсутствие адекватной коррекции возможна декомпенсация сердечной деятельности, что может приводить к неблагоприятному прогнозу лечения основного заболевания.
Пятый (V) фактор, вклад которого в прогноз ТБ у коморбидных пациентов составил 5,38%, определен как «состояние легочной функции», включает три параметра: объем форсированного выдоха (ОФВ1) за 1-ю секунду (л); ОФВ1 (%); форсированная жизненная емкость легких (ФЖЕД, л). Вентиляционная способность легких определяет доставку кислорода ко всем органам и тканям, предупреждая развитие гипоксии. Снижение функции внешнего дыхания пациентов с коморбидной бронхолегочной патологией ухудшает прогноз при ТБ.
Шестой (VI) фактор с вкладом в прогноз ТБ у коморбидных больных 5,15% определен как «центральная гемодинамика», его параметры: средняя частота сердечных сокращений; величина утреннего подъема САД.
Седьмой фактор (VII) с вкладом 4,97% включает два параметра: суточный индекс САД и суточный индекс ДАД.
Восьмой фактор (VIII) с вкладом 3,89% может быть отнесен к особенностям туберкулезного процесса и включает два параметра: форма ТБ и внелегочная локализация ТБ.
Девятый фактор (IX) с вкладом 3,65% нами обозначен как «осложнения течения ТБ», он включает формирование туберкуломы; оперативное лечение.
Десятый фактор (X) с вкладом 3,4% показывает связь между наличием распада легочной ткани и неблагоприятным исходом течения туберкулезного процесса. Фактор также включает два переменных параметра: фазу туберкулезного процесса и распад легочной ткани.
Одиннадцатый (XI) фактор с вкладом 3,34 % обозначен как «лекарственная устойчивость микобактерий ТБ». Фактор включает переменную: наличие множественной лекарственной устойчивости микобактерий туберкулеза (МЛУ).
Двенадцатый фактор (XII) с вкладом 3,13% связан с исходом лечения ТБ. Фактор включает единственную переменную: режим химиотерапии. Фактор может быть отнесен к медикаментозно корригируемым.
Тринадцатый фактор (XIII; 2,92%) – «насосная функция сердца». Фактор включает одну переменную: трансмитральный градиент, который также может быть отнесен к факторам, характеризующим состояние сердечно-сосудистой системы.
Четырнадцатый фактор (XIV; 2,82%) также относится к состоянию центральной гемодинамики, включает скорость утреннего подъема САД.
Пятнадцатый фактор (XV; 2,65%) – содержит один параметр: транспульмональный градиент и также относится к состоянию сердечно-сосудистой системы.
Шестнадцатый фактор (XVI; 2,63%) характеризует легочную функцию, содержит параметр ОФВ1/ФЖЕЛ.
Семнадцатый фактор (XVII; 2,32%) определяет состояние правых отделов сердца, содержит один параметр – размеры правый желудочек по результатам ЭхоКГ.
Обсуждение
Все анализируемые медицинские параметры можно объединить в несколько групп по степени влияния на прогноз исхода лечения ТБ.
Наибольший вклад в прогноз исхода лечения ТБ внесли факторы, характеризующие состояние центральной гемодинамики. Их общий вклад (I, IV, VII, XIV) составляет 29,03% (объединяет показатели СМАД). Эту группу можно определить как медицинскую корригируемую, она включает основные данные СМАД, что определяет состояние системы кровообращения и эластичности артерий. Данные факторы могут контролируваться отдельными группами гипотензивных препаратов.
На втором месте по степени влияния на исход лечения ТБ занимает группа факторов, характеризующих особенности туберкулезного процесса с общим вкладом 24,76%, которая объединяет II, VIII, IX, X, XI, XII факторы (локализация, распространенность, форма туберкулеза, режим химиотерапии).
Далее следует состояние насосной функции сердца, суммарно степень влияния составляет 19,5% (изменение структуры и функции сердца), оценено по данным ЭхоКГ, объединяет III, IV, XIII, XV, XVII факторы. Нами данные факторы были расценены как частично медицински корригируемые. Часть показателей, по данным ЭхоКГ, такие как трансмитральный, транспульмональный градиенты давления при проведении адекватной антиишемической и кардиопротективной терапии, могут корригироваться с восстановлением функции сердца и улучшением динамических показателей.
Наименьшее влияние на прогноз лечения ТБ оказывает группа показателей, характеризующих функцию внешнего дыхания, объединющая V и XVI факторы с суммарным влиянием 8,01% и определяемая показателями спирометрии (ОФВ1, ФЖЕЛ и ОФВ1/ФЖЕЛ). Эти показатели также могут быть отнесены к частично корригируемым, что и определяет необходимость коррекции бронхообструктивного синдрома у пациентов с ТБ и ХОБЛ [16–19]. При полноценной индивидуализированной медикаментозной бронхолитической терапии возможно улучшение функции легких, что позволяет улучшать ее и снижать вероятность неблагоприятного исхода лечения ТБ у коморбидных пациентов.
Заключение
Исходя из результатов ФА в качестве клинических предпосылок развития неблагоприятного исхода лечения у пациентов с ХОБЛ были выделены наиболее важные управляемые характеристики для осуществления эффективных профилактических мероприятий:
1. Факторы сердечно-сосудистой коморбидности – состояние центральной гемодинамики (сосудистые корригируемые терапевтически) и насосной функции сердца.
2. Туберкулезные корригируемые факторы – распространенность процесса, наличие распада, степень бактериовыделения, выделение лекарственно-устойчивых форм микобактерий ТБ, связанных с основным заболеванием, ухудшающих исходы лечение ТБ, которые также могут быть скорригированы с помощью изменения режима химиотерапии с учетом лекарственной устойчивости или продолжительности фазы лечения коморбидных пациентов.
3. Функциональные пульмонологические, корригируемые терапевтические показатели функции внешнего дыхания, определяющие состояние бронхолегочной системы. Проведение адекватной индивидуализированной бронхолитической терапии пациентов с ХОБЛ и ТБ позволит улучшить прогноз лечения ТБ.
Таким образом, в группу риска по развитию неблагоприятного исхода лечения ТБ среди коморбидных пациентов с ХОБЛ входят лица с нестабильным или повышенным систолическим, диастолическим или пульсовым давлением, при наличии гипертрофии задней стенки левого желудочка, мезжелудочковой перегородки, правого желудочка со снижением трансмитрального и транспульмонального градиента и сниженной функцией внешнего дыхания. При развитии ТБ у них процесс может становиться распространенным и можно ожидать худшего исхода лечения основного заболевания.
Возможно, в современном обществе исходы ТБ будут зависеть от коморбидности, а не от тяжести течения ТБ. Индивидуальный подбор и наличие большого количества препаратов позволяют подавлять активность МБТ даже при наличии множественной лекарственной устойчивости in vitro, но, несмотря на это, у части пациентов может быть неблагоприятный прогноз, что определяется индивидуальной реакцией на лечение и состоянием макроорганизма.
Профилактические мероприятия должны включать обязательную коррекцию бронхолегочной и сердечно-сосудистой патологии с привлечением профильных специалистов (кардиологов, пульмонологов, терапевтов) в период лечения ТБ.
Вклад авторов. Концепция и дизайн исследования – Н.В. Багишева, А.В. Мордык. Сбор и обработка материала – А.Р. Ароян, С.А. Руденко, Н.В. Ширинская. Статистическая обработка – В.В. Гольтяпин. Написание текста – Н.В. Багишева, А.В. Мордык. Редактирование – А.В. Мордык, И.А. Викторова, К.И. Нестерова.