Введение
К концу XIX в. в мире развился интерес к лечению психических заболеваний в общей медицине, психиатрические отделения появились в больницах общего профиля и началось обучение врачей и студентов диагностике и лечению психических нарушений у физически больных пациентов [1]. Тем не менее отношение к возможному появлению врача-психиатра в медицинском отделении больницы варьировалось от враждебного до безразличного. В 1929 г. психиатр Дж. Генри [2] документально описал свой профессиональный опыт. В той статье он сообщил о 300 случаях выявления и диагностики психиатрического расстройства у больных соматической патологией. Несмотря на изменения в диагностической терминологии и дифференциальных критериях, полученные данные обнаруживают сходство с современными научными представлениями. Опыт оказания стационарной помощи в психиатрических учреждениях больным соматическими заболеваниями, а также в рамках психиатрических консультаций пациентов в отделениях общего профиля положил начало направлению консультативно-междисциплинарной психиатрии, которая занималась изучением и коррекцией психологических изменений у пациентов с соматическими заболеваниями.
Развитию психических расстройств у онкологических больных способствуют несколько факторов. С одной стороны, это стресс, связанный с выявлением онкологического заболевания, ожиданием мучений и физически калечащего лечения. С другой – улучшение непосредственных результатов противоопухолевого лечения приводит к тому, что некоторые злокачественные заболевания приобретают черты хронических, с длительными периодами ремиссий и периодическими «обострениями» (рецидивами или прогрессированием). В результате могут появляться проблемы, связанные с психическим функционированием и выработкой адаптивных стратегий, свойственных пациентам с длительно существующими, потенциально инвалидизирующими и фатальными хроническими заболеваниями. Одновременно с этим в связи с общей гуманизацией современного общества увеличивается внимание и к практическим вопросам качества жизни пациентов и членов их семей, в немалой степени связанным с психологическим и психиатрическим здоровьем.
Психоонкология
Психоонкология – направление психиатрии, активно развивающееся в последние несколько лет в связи с необходимостью выявления как откровенных психических расстройств, так и коррекции неадекватных, дезадаптивных реакций на онкологическое заболевание, способствует улучшению результатов противоопухолевого лечения и повышению качества жизни пациентов.
Признание и обращение к психиатрическим симптомам у онкологических пациентов служат относительно недавним направлением в медицине, активно развивающимся с 1970-х гг. [3]. В результате в развитых странах онкологические пациенты с симптомами психических расстройств в настоящее время естественным образом попадают в сферу интересов психоонкологов, специфической особенностью работы которых считается учет потенциальных взаимодействий лекарственных препаратов, используемых в психиатрии и онкологии; необходимость дифференцировать клинически схожие симптомы и побочные эффекты противоопухолевого и психиатрического лечения и определение целесообразности применения психофармакологических средств по непсихиатрическим показаниям.
Психическое расстройство может присутствовать у пациента независимо от онкологического заболевания. Иногда у пациентов, получающих лечение или наблюдающихся по поводу психиатрических заболеваний, развиваются злокачественные новообразования. Во всяком случае распространенность онкологических заболеваний у пациентов с шизофренией, биполярным расстройством или злоупотреблением психоактивными веществами не ниже, чем в общей популяции. Коморбидность шизофрении и расстройств шизофренического спектра с онкологическими заболеваниями в России достаточно высока – 3,2 и 4,1% соответственно [4]. Шизофрения и расстройства шизофренического спектра могут оказывать значимое влияние на процессы диагностики и лечения онкологического заболевания. Такие больные не всегда своевременно обращаются за медицинской помощью, часто игнорируют выявленное онкозаболевание, отказываясь выполнять рекомендации специалистов, проявляют повышенную тревожность, требуя медицинских необоснованных дополнительных обследований, нарушают режим противоопухолевой терапии, обнаруживают аномальные формы поведения в условиях онкологического стационара.
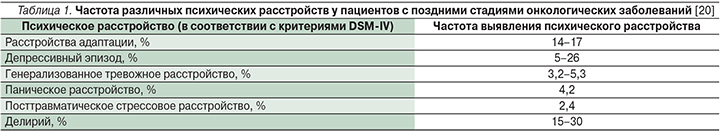
Психопатологические реакции у онкологических больных присутствуют чаще, чем в общей популяции. Одним из первых психиатрический подход к диагностике расстройств у онкологических пациентов без ранее выявленной эндогенной психиатрической патологии применил A.M. Sutherland [5]. Он описал несколько клинических типов психологических и психопатологических реакций, появление которых наблюдал у пациентов сразу после того, как им устанавливали диагноз злокачественного новообразования, так и в процессе противоопухолевого лечения: зависимость от окружающих, тревогу, послеоперационную депрессию, ипохондрический ответ, обсессивно-компульсивные реакции и параноидные реакции. A.M. Sutherland отмечал, что онкологические больные находятся в состоянии специфической тяжелой формы стресса, для которой свойственна актуализация фундаментальных убеждений, основанных на жизненной истории и личном опыте. Последующие исследования подтвердили наличие, распространенность, необходимость диагностики и коррекции психосоциальных расстройств, особенно тревоги и депрессии, у онкологических больных на разных стадиях заболевания [6–8]. Конкретные диагностические критерии, позволяющие фиксировать психические расстройства, связанные с диагностикой и лечением онкологических заболеваний, были введены в DSM (Diagnostic and Statistical Manual of mental disorders) начиная с его 3-й редакции [9]. В первом многоцентровом исследовании распространенности психических расстройств среди онкологических больных PSYCOG, проведенном в США и опубликованном в 1983 г., показано, что почти 50% онкологических больных соответствовали критериям диагнозов DSM-III (преимущественно в связи с расстройствами адаптации) [10]. Похожие результаты в последующем были получены как в аналогичных исследованиях, проведенных в отдельных странах: Великобритании, Бельгии, Италии, Австралии, Испании, Германии [11–17], так и в мета-анализах исследований [18–20]. Все исследования независимо от использованных критериев психических расстройств (DSM или Международной классификацией болезней Всемирной организации здравоохранения) показали, что по крайней мере один из трех пациентов, страдающих онкологическими заболеваниями, имеет симптомы, указывающие на психическое расстройство. В отечественной психиатрии имеются данные о значительном превышении уровня психической патологии у больных злокачественными новообразованиями по сравнению с населением и преобладаниями нозогенных реакций (расстройств адаптации) в спектре психических нарушений в рассматриваемом контингенте пациентов [21]. Типы нозогений и их дальнейшее развитие зависят от локализации опухоли (например, при раке поджелудочной железы риск депрессивных расстройств увеличивается), стадии заболевания (при поздних стадиях чаще встречается делирий) и условий лечения (при амбулаторном лечении психические расстройства возникают реже, чем у госпитализированных больных или пациентов хосписов). В целом в течение онкологического заболевания преобладают депрессивные, тревожно- и стресс-ассоциированные расстройства, но частота их выявления и выраженности увеличивается на поздних стадиях болезни; табл. 1.
В клинической практике в отсутствие законодательных ограничений психотропные препараты часто назначают онкологическим пациентам. По результатам обсервационных исследований последних 35 лет выявлено частое и обоснованное назначение психотропных препаратов онкологическим больным. В одном из первых сообщений по этой теме L.R. Derogatis et al. [22] указали, что психотропные препараты получали более половины из 1579 обследованных больных опухолевыми новообразованиями, в т.ч. снотворные (48% от общего числа рецептов), антипсихотики (26%), анксиолитики (25%) и антидепрессанты (1%). Аналогичные данные были представлены в последующем H. Jaeger et al. [23], которые обнаружили, что пациентам с распространенными опухолями чаще всего назначались антипсихотические средства (в 61,3%) и гипнотики (в 55,8%). Они отметили возрастающее число назначений антидепрессантов (10% случаев). Чаще всего поводом к назначению психотропных препаратов служили расстройства сна, тошнота и рвота. F.C. Stiefel et al. [24], анализировавшие назначение психотропных препаратов онкологическим пациентам на протяжении 10-летнего периода, отметили тенденцию изменения спектра их назначения с постепенным увеличением доли антидепрессантов; кроме того, психотропные препараты на протяжении периода исследования стали использоваться по более широким показаниям при относительно стабильных нормах отпуска по каждому рецепту для разных классов психотропных препаратов. По-видимому, этому способствовало появление новых эффективных и относительно безопасных лекарственных средств, в т.ч. антидепрессантов последнего поколения (селективных ингибиторов обратного захвата серотонина [СИОЗС] и селективных ингибиторов обратного захвата норадреналина [СИОЗН], в последующем и селективных ингибиторов обратного захвата серотонина и норадреналина [СИОЗСиН]), изменяющее предпочтения врачей в отношении их назначения онкологическим больным. В последнее время показания к назначению психотропных препаратов в онкологии еще более расширились и включают как симптомы опухолевого заболевания, так и индуцированные лечением жалобы: приливы, невропатическую боль, тошноту, рвоту, слабость, хроническую усталость, зуд и т.д. [25, 26]. Растет и доля онкологических пациентов, получающих психотропные препараты. С. Farriols et al. [27], отслеживавшие динамику назначений психотропных препаратов на протяжении 7 лет (2002–2009; 840 включенных в исследование пациентов), отметили увеличение использования антипсихотических препаратов, особенно галоперидола и рисперидона (с 26,1 до 40%), антидепрессантов, в т.ч. миртазапина, циталопрама, эсциталопрама и дулоксетина (с 17,8 до 27,1%), бензодиазепинов, особенно лоразепама и мидазолама (с 72,6 до 84%). Важным показанием к назначению психотропных препаратов служат психоэмоциональные нарушения, распространенность которых у онкологических больных довольно высока. В исследовании, включившем 7298 онкологических и 14 596 неонкологических пациентов, частота эмоциональных расстройств составила 15,6 и 1,4% соответственно. Не вызывает удивления, что онкологические пациенты получали психотропные препараты (анксиолитики и антипсихотики) чаще и дольше [28]. Аналогичные данные результатов сравнительного исследования женщин, получавших лечение в связи с различными заболеваниями молочных желез (всего более 10 тыс. пациенток, в т.ч. более 2000 со злокачественными новообразованиями), представили G.H. De Bock et al. [29] Очевидна и оправданна тенденция более частого назначения психотропных препаратов при поздних стадиях онкологического заболевания, особенно незадолго до смерти [30]. По результатам исследования DELPHI (опрос 135 ведущих специалистов по паллиативной помощи из девяти стран) антипсихотики и транквилизаторы вошли в список четырех основных групп лекарственных средств, которые должны быть обязательно доступны для онкологических пациентов в рамках паллиативной помощи [31].
Однако в психотропных препаратах могут нуждаться не только пациенты, получающие противоопухолевое лечение, но и успешно излеченные. Повышенная вероятность использования всех категорий антидепрессантов была выявлена у взрослых, успешно излеченных от онкологических заболеваний в детстве, по сравнению со здоровыми лицами [32].
Порядок, алгоритмы и рекомендации назначения психотропных препаратов у онкологических больных
К настоящему времени доступны руководства по наиболее эффективному лечению всех основных психических расстройств онкологических пациентов, в т.ч. делирия [31, 33], депрессии, выявленные в процессе активного противоопухолевого лечения [34, 35], и депрессии, развивающейся при паллиативной помощи [36]. В связи с тем что последние недели жизни инкурабельных онкологических пациентов часто омрачаются тяжелыми симптомами страдания (в т.ч. чрезмерной тревогой, болью, одышкой, тошнотой, беспокойством и ажитированным делирием), разработано несколько паллиативных седативных протоколов конца жизни [37–39].
Избранные вопросы клинического использования психотропных препаратов
Клиническое применение психофармакологических средств в онкологии в последние годы значительно возросло. Использование психотропных препаратов в онкологических клиниках и стационарах паллиативной помощи в развитых странах стало обязательным и повсеместным компонентом комплексной программы лечения и реабилитации [40]. При этом обязательным условием рационального назначения психофармакологических средств служат анализ противоопухолевой терапии, получаемой пациентом, и возможность назначения психотропных препаратов для лечения психических симптомов с учетом фармакокинетики и конкурентного взаимодействия всех лекарственных средств, получаемых больным [41]. Основные группы психотропных препаратов и область их применения в онкологии приведены в табл. 2.

В настоящее время в онкологии психотропные препараты широко используются не только в связи с психиатрическими показаниями, но и для коррекции непсихиатрических симптомов: боли, приливов, потери аппетита и усталости [39].
Антидепрессанты. Европейское общество медицинской онкологии (ESMO) рассматривает антидепрессанты как возможный компонент лечения болевого синдрома вообще и необходимый компонент обезболивания онкологических больных на поздних стадиях болезни [42]. В комплексной терапии болевого синдрома предпочтение отдается селективным ингибиторам обратного захвата серотонина и норадреналина [43]. Также широко используются антидепрессанты и при лечении вторичных приливов, особенно при гормональной терапии рака молочной железы блокаторами рецепторов эстрогена (тамоксифен) или ингибиторами ароматазы (летрозол, анастрозол, экземестан) [44]. Антигистаминовая активность некоторых антидепрессантов используется в лечении тошноты и синдрома анорексии-кахексии, вызванных химиотерапией [45, 46]. Кроме того, применение антидепрессанта бупропиона снижает выраженность хронической усталости, одного из специфического синдрома онкологических больных [47, 48].
Психостимуляторы. Психости-муляторы уменьшают выраженность хронической усталости [47, 48], положительно влияют на качество жизни, активируя психические функции, повышая физическую активность, улучшая способность к концентрации внимания, вигильность и инициативность [49, 50].
Антипсихотики и транквилизаторы. Антипсихотики (в частности, оланзопин) повышают эффективность антиэметиков при лечении тошноты и рвоты, вызванной химиотерапией. Похожие данные были получены при использовании бензодиазепинов, которые благодаря своим амнезическим свойствам могут способствовать уменьшению тошноты и рвоты, вызванных противоопухолевым лечением.
Тимометики. Противосудорожные средства первого и второго поколений, которые также используются в качестве стабилизаторов настроения (карбамазепин, топирамат, габапентин), оказались эффективными для лечения болевого синдрома при токсической невропатии [51].
Выводы
Психические расстройства распространены среди онкологических пациентов и отрицательно влияют на качество жизни. Потребность онкобольных в психосоциальной, психотерапевтической и психофармакологической помощи очевидна и востребована на протяжении всего периода заболевания и противоопухолевого лечения. Информация о наиболее важных психотропных препаратах и их правильном использовании в клинической практике имеет большое значение как для онкологов и врачей паллиативной помощи, так и для пациентов; она должна содержать не только общую характеристику лекарств, но и сведения об их взаимодействии с противоопухолевыми средствами, эффективности и безопасности при лечении психических нарушений, вторичных по отношению к раку. Вместе с тем результаты исследований и клинического опыта психоонкологии демонстрируют необходимость учета феноменологических аспектов онкологических больных, разнообразия психосоциальных расстройств и различных вариантов биологических ответов на психотропные препараты, что может быть реализовано только при тесном сотрудничестве онкологов и специалистов в области психического здоровья.


