Введение
Синкинезии – непроизвольные движения лицевой мускулатуры одной мышечной группы в ответ на произвольные движения другой мышечной группы лица, возникающие у пациентов через 4–6 месяцев в результате повреждения лицевого нерва (ЛН) [1].
В нейрохирургической практике одной из причин возникновения поражения ЛН, которое в дальнейшем приводит к формированию синкинезий, служит удаление опухолей задней черепной ямки и мосто-мозжечкового угла, в первую очередь вестибулярных шванном.
В настоящее время существует три гипотезы возникновения синкинезий. Наибольшее признание получила теория, подразумевающая, что после повреждения аксоны подвергаются аберрантной регенерации с формированием иннервации групп мышц, которые они не иннервировали ранее. Второй потенциальный патологический механизм подразумевает эфпатическую передачу сигнала, при которой рядом расположенные аксоны в области поражения стимулируют друг друга, вероятно в результате потери миелиновой оболочки. Наконец, некоторые исследования указывают на возможность наличия центрального механизма возникновения синкинезий в результате перевозбуждения двигательного ядра лицевого нерва [2].
В клинической практике чаще всего встречаются окуло-оральные (движение комиссуры рта при произвольном закрывании глазной щели) и орально-окулярные (сужение глазной щели при движении рта) синкинезии. В связи с тем что синкинезии обычно проявляются чередованием зон гипер- и гипокинезов, применяемые методы лечения должны быть направлены как на подавление чрезмерной мышечной активности в зависимости от области лица, так и на восстановление подвижности.
Такие физиотерапевтические методики, как лечебная физкультура (ЛФК), массаж, электростимуляция, весьма трудоемки и часто не приносят желаемых результатов, в т.ч. и потому, что не оказывают влияния на патологическую «цепь синкинезий» – последовательность вовлечения непроизвольных мышечных сокращений на пораженной стороне в ответ на произвольное движение [3].
Ботулинический токсин типа А (БТА) применяется для селективного подавления сократимости мышечных волокон и эффективно используется пациентами в остром и отделенном периодах поражения ЛН различной этиологии [4]. Однако число исследований его эффективности для пациентов с синкинезиями после нейрохирургического вмешательства ограниченно, что обусловило цель данной работы.
Цель исследования: оценить эффективность ботулинотерапии пациентов с синкинезиями после нейрохирургических вмешательств.
Методы
В 2013–2018 гг. проведено проспективное исследование, в которое были включены 150 пациентов с острой невропатией ЛН, возникшей после хирургического лечения опухолей задней черепной ямки и мосто-мозжечкового угла. Все пациенты разделены на две группы: I (основную) группую – 103 (68,7%) пациента (59 [57,3%] мужчин и 44 [42,7%] женщин в возрасте 43,7±9,8 года), и II (контрольную) группу – 47 (31,3%) больных (27 [57,4%] мужчин и 20 [42,6%] женщин в возрасте 46,7±10,2 года).
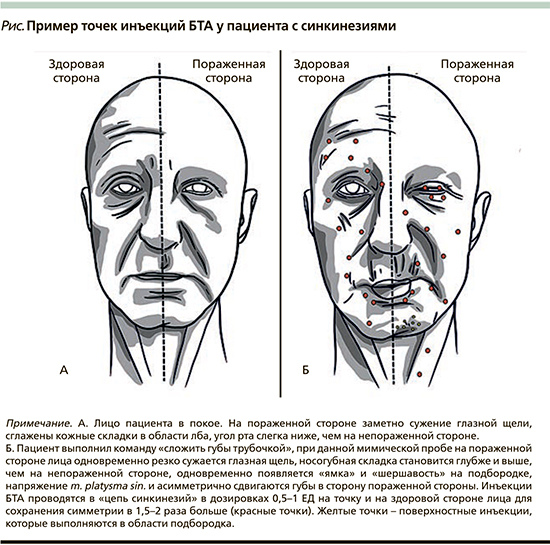
Через 5–8 месяцев после поражения ЛН при появлении синкинезий начинали лечение данного осложнения БТА (Incobotulinumtoxin A) с интервалом введения через 3 и 6 месяцев. Введение БТА осуществляли на пораженной стороне в малых дозировках (0,5–1,5 ЕД на точку) и симметрично на здоровой стороне в дозировках, в 1,5–2,0 раза превышающих аналогичные на пораженной (см. рисунок). Мышцам, наиболее часто вовлеченным в возникновение патологической синкинетической активности, таким как m. orbicularis oculi, m. zygomaticus major, m. zygomaticus minor, m. mentalis, m. platysma, m.buccinator, уделяли особое внимание при введении инъекций на стороне поражения. Остальные мышцы выбирали в зависимости от типа синкинезий и их включения в патологическую активность при движении. Пациенты контрольной группы продолжали курсы ЛФК, начатые в остром периоде, синкинезии корректировались путем выполнения специальных упражнений перед зеркалом, а также точечным массажем болезненных уплотненных мышечных тяжей.
Критерии включения пациентов в исследование: возраст 18–65 лет; наличие острого поражения ЛН, развившегося после хирургического лечения опухолей задней черепной ямки и мосто-мозжечкового угла.
Критерии невключения пациентов в исследование: несоответствие критериям включения; острое нарушение мозгового кровообращения, инфаркт миокарда, инфекционные заболевания, декомпенсация хронических заболеваний (сердечно-сосудистых, сахарного диабета); наличие психических расстройств.
Критерии исключения пациентов из исследования: поражение ЛН ненейрохирургической этиологии; нерегулярное посещение клиники для проведения контрольных исследований вследствие как объективных, так и необъективных причин; полная несохранность ЛН во время удаления опухоли.
Среди обследованных больных 122 (81,3%) были после удаления невриномы слухового нерва, из них в I группе – это 82 (79,6%), во II – 40 (85,1%) человек. После удаления других опухолей задней черепной ямки и мосто-мозжечкового угла (петрокливальная менингиома, нейрофиброма, холестеатома) насчитывалось 28 (18,7%) больных, из них 21 (20,4%) и 7 (14,9%) из I и II групп соответственно.
Эффективность лечения оценивалась клинически с оценкой жалоб, провоцирующих факторов, с применением мимических проб в покое и при произвольной активности. Для оценки симметрии лица и синкинезий использовалась Шкала Sunnybrook Facial Grading Scale (SFG). Самостоятельно пациенты заполняли шкалу FDI (Facial Disability Index). Продолжительность исследования составила 2 года.
Статистический анализ
Статистическая обработка результатов исследования проведена с использованием Microsoft Excel и статистического программного обеспечения SPSS 23.0 и Statistica 8.0 for Windows (StatSoftInc., USA). Различия считались статистически значимыми при уровне ошибки p<0,05.
Результаты
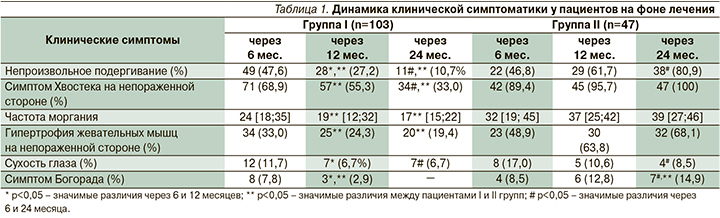
Через полгода после поражения ЛН синкинезии, значимо ухудшавшие качество жизни пациентов, выявлены у 48 (46,6%) и 30 (63,8%) пациентов I и II групп соответственно, через год – у 28 (27,2%) и 32 (68,1%; p<0,001) и через 2 года – у 14 (13,6%) и 40 (85,1%; p<0,001) пациентов.
Для большинства пациентов как I, так и II группы (n=45 [93,8%] и n=27 [90,0%]) в «цепь синкинезий» (последовательность вовлечения непроизвольных мышечных сокращений на пораженной стороне в ответ на произвольное движение) преимущественно были вовлечены скуловые мышцы, круговая мышца глаза и рта, подбородочная мышца, подкожная мыщца шеи. Синкинезии наблюдались при проведении мимических проб, а также при нагрузке (жевание, улыбка, зевание, прищуривание).
Оценка динамики клинической симптоматики в течение 24 месяцев наблюдения выявила снижение основных симптомов в группе пациентов, лечение которых продолжалось с использованием БТА, тогда как у пациентов группы сравнения отмечено их увеличение. Так, в I группе число пациентов с симптомом Хвостека на непораженной стороне уменьшилось в 1,60 раза – с 6-го по 12-й месяц исследования (p<0,05), и в 2,68 раза – с 6-го по 24-й месяцы наблюдения (p<0,01), тогда как во II группе через 6 месяцев исследования пациентов, у которых выявлялся данный симптом, было значимо больше (в 1,30 раза; p<0,05), а через 24 месяца он выявлялся уже у всех пациентов данной группы.
Частота моргания также постепенно снижалась у пациентов I группы и стала нормальной у большинства пациентов к 24-му месяцу наблюдения, тогда как во II группе она повышалась (p>0,05). Гипертрофия жевательных мышц на непораженной стороне, связанная с тем, что на ней пациенты в большей степени пережевывали твердую пищу, уменьшилась в 1,70 раза в I группе пациентов (p<0,05) к 24-му месяцу исследования (по сравнению с 6-м месяцем), а во II группе, наоборот, увеличилась в 1,40 раза (p<0,05). Симптом Богорада (моторно-вегетативная синкинезия) к 24-му месяцу наблюдения отсутствовал у пациентов I группы, тогда как во II выявлялся в 19,3% наблюдения (p<0,05; табл. 1).
Уже через 6 месяцев после поражения ЛН общее состояние лицевой мускулатуры у пациентов I группы, оцененное с использованием шкалы Sunnybrook Facial Grading System, было в 2,0 раза лучше, чем у пациентов II группы (p<0,01). Важно отметить, что по всем подшкалам (симметрия покоя, симметрия произвольных движений и синкинезии) показатели пациентов I группе были лучше, чем II.
Через 12 месяцев у пациентов I группы общее состояние лицевой мускулатуры было в 2,3 раза лучше, чем во II группе (p<0,01), данная тенденция сохранилась и через 2 года с момента начала исследования, когда состояние мимических мышц у пациентов I группы было лучше, чем во II, в 1,68 раза (p<0,05; табл. 2).
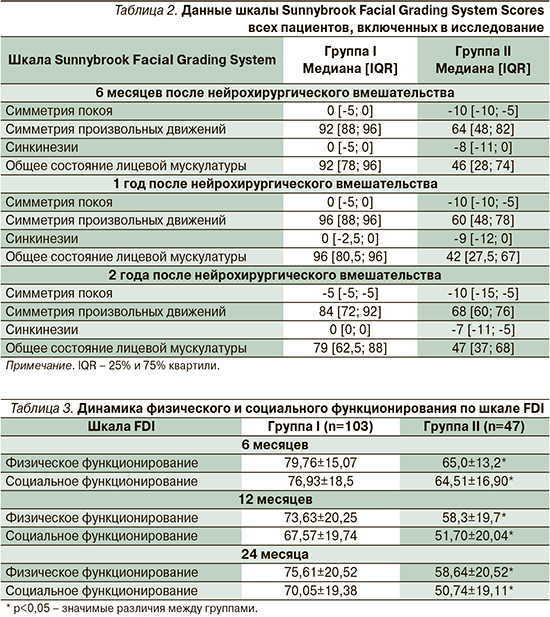
Через 6 месяцев после начала исследования качество жизни как в отношнии физического, так и социального функционирования пациентов II группы было в 1,23 и 1,19 раза хуже по сравнению с пациентами I группы. Через 12 месяцев данные показатели были в 1,26 и 1,31 раза ниже у пациентов II группы, через 24 месяца – в 1,29 и 1,38 раза соответственно (табл. 3).
Обсуждение
БТА уменьшает выраженность синкинезий на пораженной стороне, но для сохранения симметрии лица необходимо введение препарата и в здоровую сторону. Такое введение препарата способствует постепенному улучшению контроля тонких мимических движений и мышечной силы на стороне поражения [5, 6].
В проведенном исследовании показана эффективность введения БТА с двух сторон для лечения синкинезий, оцениваемая у пациентов с хроническими последствиями поражения ЛН с применением шкалы Sunnybrook и динамической оценки асимметрии лица, которые продемонстрировали, что после введения БТА на стороне поражения и контралатеральной стороне у пациентов наблюдалось значимое подавление синкинезий, улучшение симметрии лица как в покое, так и при мимических движениях в сочетании с улучшением качества жизни, социальных взаимодействий, восприятия собственного внешнего вида.
Проведенное исследование позволило нам сформулировать основные принципы введения БТА пациентам с синкинезиями:
- Выбор мышцы в зависимости от типа синкинезий и их включения в патологическую активность.
- Введение БТА в «цепь синкинезий».
- Введение БТА на пораженной стороне в малых дозировках (0,5–1,5 ЕД на точку).
- Симметричное введение БТА на здоровой стороне для сохранения симметрии лица в дозировке, в 1,5–2,0 раза превышающей аналогичные на пораженной.
- Осторожность с мышцами средней половины лица (m. zygomaticus major и m. zygomaticus minor).
- Рекомендации после инъекции – не лежать 2 часа, мимическая активность – 15–30 минут.
Заключение
Дифференцированное применение ботулинотерапии в качестве коррекции синкинезий необходимо для эффективного восстановления функций мимических мышц после нейрохирургических вмешательств при опухолях задней черепной ямки и мосто-мозжечкового угла. При синкинезиях ботулинотерапия показана с двух сторон, при этом доза препарата на пораженной стороне должна составлять от 1/2 до 1/3 от здоровой стороны. Процедуры должны проводиться регулярно – в среднем 1 раз в 3 месяца. Возможно этапное проведение процедур в оставшиеся зоны синкинезий в зависимости от клинического эффекта.
Вклад авторов
Концепция и дизайн исследования – О.Р. Орлова, М.А. Акулов.
Сбор и обработка материала – С.В. Таняшин, М.А. Акулов.
Статистическая обработка данных – А.С. Орлова.
Написание текста – В.Н. Шиманский, В.О. Захаров, П.Н. Яковлева.
Редактирование – О.Р. Орлова, М.А. Акулов.