Введение
Хроническая обструктивная болезнь легких (ХОБЛ) – заболевание, которое характеризуется прогрессирующим воспалением дыхательных путей с постепенным ограничением воздушного потока за счет воздействия внешних патогенных факторов. ХОБЛ становится третьей по значимости причиной смертности среди людей во всем мире после сердечных заболеваний и инсульта [1]. Распространенность ХОБЛ в мире у людей старше 40 лет составляет от 10,1 до 15,8% [2]. Смертность от ХОБЛ с 1990 г. увеличилась на 12% [1–3].
Тема хронической бронхолегочной патологии актуальна еще по причине сохранения резервуара туберкулезной инфекции [4]. Туберкулез (ТБ) остается глобальной проблемой здравоохранения и затрагивает 8,8 млн человек ежегодно. С одной стороны, растет число случаев с множественной лекарственной устойчивостью [5, 6], с другой стороны, не менее актуально сочетание ХОБЛ и ТБ [7–9]: до трети пациентов с ТБ имеют ХОБЛ, поэтому понимание особенностей ведения пациентов данной категории актуально как для фтизиатрии, так и для пульмонологии [4]. Признаны общие факторы риска для обоих заболеваний: курение, ухудшение состояния иммунной системы. ТБ легких может повышать вероятность последующего развития ХОБЛ даже после завершения эффективного лечения ТБ, а ХОБЛ утяжеляет течение ТБ. Наблюдается двунаправленная связь между этими заболеваниями легких, где каждое может выступать в качестве независимого фактора риска для другого, что имеет важные последствия для соответствующего долгосрочного лечения ТБ и ХОБЛ [10–13].
Бронхообструктивный синдром (БОС) различной степени тяжести встречается практически при всех формах ТБ легких, частота его выявления зависит от длительности течения специфического процесса и от выраженности остаточных изменений в легких [14–16]. Клинические особенности ХОБЛ могут способствовать длительному хроническому течению ТБ, а ТБ в свою очередь практически всегда сопровождается развитием БОС. При сочетанной патологии следует рассматривать комплексный подход к улучшению контроля и управления общими условиями, факторами риска, влияющими на развитие обоих заболеваний [17, 18], для улучшения качества жизни и прогноза лечения для пациентов данной категории.
Помимо функции дыхания ХОБЛ следует оценивать на основе симптомов, частоты и тяжести обострений и качества жизни, связанного со здоровьем [19]. Терапия БОС направлена на повышение толерантности к физической нагрузке и снижение одышки, улучшение повседневной деятельности. Это может быть достигнуто путем подбора лекарственных средств для снижения выраженности одышки, гиперинфляции, частоты и тяжести обострения. Все рекомендации приводят бронходилататоры в качестве базисной терапии для всех этапов ХОБЛ. К ним относятся длительно действующие β2-агонисты (ДДБА), длительно действующие антихолинергики (ДДАХ), наиболее эффективные при регулярном лечении в клинически стабильной фазе. Эффективность бронходилататоров должна оцениваться с точки зрения функциональности (облегчение бронхиальной обструкции и легочной гиперинфляции), симптоматического (толерантность к физической нагрузке, выраженность одышки), а также клиническое улучшение (уменьшение числа или тяжести обострений) [19–21].
Терапия ХОБЛ четко прописана в GOLD-2020 [1] и Федеральных клинических рекомендациях [22]. В качестве первой линии терапии рассматриваются β2-агонисты и антихо-линергические препараты длительного действия. Ингаляционная терапия предпочтительнее других методов введения препаратов. При легкой степени обычно назначают короткодействующие препараты по потребности, при среднетяжелой – постоянное применение одного или двух бронхолитических препаратов (в зависимости от эффективности), при тяжелой и крайне тяжелой – комбинированное применение бронходилататоров с модификацией методов их доставки (спейсеры, небулайзеры), присоединением ингаляционных и системных глюкокортикостероидов, рофлумиласта [20, 21].
β2-агонисты характеризуются быстрым началом действия и достаточной продолжительностью, но с возрастом количество β-рецепторов уменьшается, следовательно, и эффект от препаратов будет снижаться, не исключено развитие с возра-стом аритмогенного действия препаратов данной группы. Олодатерол является представителем агонистов β2-адренорецепторов длительного действия с однократным применением в течение суток. Профиль безопасности ДДБА сопоставим с плацебо [20].
Антихолинергические препараты, несмотря на то что эффект от их применения развивается несколько дольше, имеют ряд преимуществ, что делает их оптимальными для применения некоторыми категориями пациентов, в частности ТБ+ХОБЛ. Они не обладают кардиотоксичностью, не развивается привыкания, нет снижения чувствительности к препаратам с возрастом, возможен ингаляционный длительный прием без развития побочных эффектов. Антихолинергические препараты обладают пролонгированным действием до 24 часов, что позволяет использовать их 1 раз в сутки, повышая приверженность пациентов лечению. Тио-тропия бромид (Тб) – четвертичное аммониевое соединение, селективен для М1- и М3-ХР, 24-часовой продолжительности действия, существует в двух формах для ингаляционного применения: порошок в капсулах 18 мкг для использования с помощью хандихалера и раствор 2,5 мкг для использования с помощью дозирующего устройства респимат [21].
В настоящее время особый интерес представляют комбинированные препараты ДДАХ/ДДБА, объединяющие положительные эффекты препаратов двух различных групп, обеспечивают бронхорасширяющий эффект за счет воздействия на различные механизмы, при низких дозах препаратов достигается минимизация побочных эффектов. В связи с вышеизложенным считаем актуальным изучение эффективности включения Тб и тиотропия бромида/олодатерола (Тб/О) в комплексную терапию пациентов с ТБ+ХОБЛ, нуждающихся в медикаментозной коррекции БОС [8, 19, 22, 23].
Цель исследования: провести сравнительный анализ эффективности использования Тб и Тб/О в качестве терапии сопровождения для коррекции БОС у пациентов с коморбидной патологией ТБ+ХОБЛ.
Методы
Проведено простое проспективное сравнительное исследование, в которое были включены 62 пациента. Критерии включения: впервые выявленный ТБ легких, наличие ХОБЛ различной степени тяжести, обязательное выполнение рентгенографии или мультиспиральной компьютерной томографии органов грудной клетки, спирометрии, информированное согласие на участие в исследовании, возраст от 40 до 80 лет. Критерии исключения: возраст моложе 40 и старше 80 лет, отсутствие сопутствующей ХОБЛ, отсутствие спирометрии, подтверждающей наличие ХОБЛ, несогласие пациентов на участие в исследовании. В соответствие с критериями включения на данном этапе в исследование взяты 62 пациента с ТБ+ХОБЛ в возрасте от 40 до 75 лет, Me (25;75) 58,0 (48,0;65,0) лет. Среди включенных в исследование преобладали мужчины – 33 (53,2%) человека, 29 (46,8%) женщин. Распределение пациентов по формам ТБ представлено на рис. 1.
Инфильтративный ТБ был у 56 (90,3±3,8%) больных, очаговый ТБ – у 3 (4,8±2,7%) , фиброзно-кавернозный ТБ – у 2 (3,2±2,2%) , диссеминированный ТБ – у 1 (1,6±1,6%) больного. Пациенты получали лечение по I и III режимам химиотерапии.
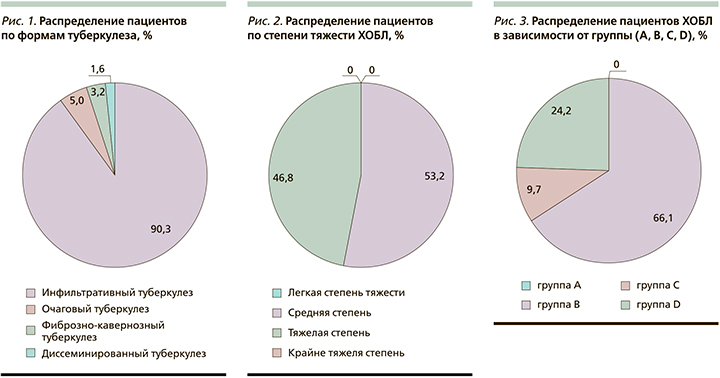
ХОБЛ в группе исследования средней степени тяжести была у 33 (53,2±6,3%) пациентов, тяжелой степени – у 29 (46,8±6,3%) больных, легкой и крайне тяжелой степени не было (рис. 2).
Распределение пациентов с ХОБЛ по группам в зависимости от выраженности симптомов и числа обострений в год представлено на рис. 3.
По категориям пациенты с ХОБЛ распределились следующим образом: В – 41 (66,1±6,0%), С – 6 (9,7±3,8%), D – 15 (24,2±5,4%) пациентов, пациентов группы А среди включенных в исследование не было.
В зависимости от характера бронхолитической терапии включенные в исследование пациенты были разделены на две группы: группа 1 (n=31) одновременно с химиотерапией ТБ по поводу ХОБЛ получали ДДАХ (Тб) в устройстве хандихалер 18 мкг 1 раз в сутки или респимат 2,5 мкг 2 дозы 1 раз в сутки, пациенты группы 2 (n=31) получали ДДАХ/ДДБА (Тб/О) в устройстве респимат 2,5/2,5 мкг 2 дозы 1 раз в сутки. Возраст Me (25; 75) пациентов группы 1 составил 62,0 (53,0; 74,0), группы 2 – 63,0 (56,0; 77,0) года. Все пациенты получали параллельно с химиотерапией ТБ бронхолитическую терапию в течение 3 месяцев в период стационарного лечения в противотуберкулезном диспансере. Контроль приема препаратов (техника ингаляции и регулярность приема) осуществлялась средним медперсоналом диспансера.
Всем пациентам проводилась оценка клинических данных (одышка по mMRC-шкале – modified Medical Research Council, САТ-тест – COPD Assessment Test) и спирометрическое исследование с оценкой ОФВ1 (объем форсированного выдоха за первую секунду, л), ОФВ1 (%), постбронходилатационный тест ОФВ1/ФЖЕЛ (форсированная жизненная емкость легких) в начале терапии и через 3 месяца регулярного приема бронхолитических препаратов.
Статистическая обработка данных была проведена с использованием пакетов программ Statistica 8.0: рассчитывали показатели описательной статистики, достоверность различий показателей в группах определяли с помощью χ2-критерия, для сравнения количественных данных в группах применяли критерий Манна–Уитни.
Результаты исследования
Была оценена динамика основных клинических и спирометрических показателей в группах сравнения за 3 месяца (табл. 1) на фоне различных вариантов бронхолитической тера-пии.
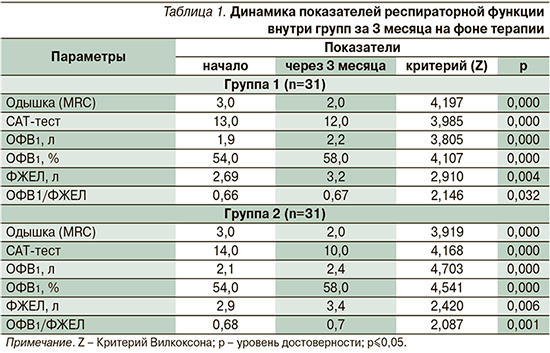
По результатам наблюдения в обеих группах наблюдалась положительная динамика всех изучаемых переменных на фоне бронхолитической терапии у пациентов ТБ+ХОБЛ, оцениваемая по выраженности одышки, САТ-тесту, по показателям спирометрии. На фоне каждого препарата достигнуто статистически значимое уменьшение одышки (на 1 балл) по MRC шкале за 3 месяца – с 3,0 до 2,0 баллов на фоне ДДАХ (Тб) (Z=2,19; p=0,000) и ДДАХ/ДДБА (Тб/О) (Z=3,92; p=0,000) соответственно. Прирост ОФВ1 за 3 месяца терапии при приеме ДДАХ (Z=3,81;p=0,000) и ДДАХ/ДДБА (Z=4,70; p=0,000) составил 300 мл в группах соответственно. По САТ-тесту на фоне приема ДДАХ отмечено снижение на 1 балл (с 13,0 до 12,0 баллов) (Z=3,985; p=0,000), в группе ДДАХ/ДДБА на 4 балла (с 14,0 до 10 баллов) (Z=4,168; p=0,000). Следовательно, двойной бронхолитик оказался эффективнее монотерапии ДДАХ по субъективному восприятию пациентов (табл. 2).
При сравнении анализируемых переменных на фоне моно- и комбинированной бронхолитической терапии получено статистически значимое преимущество по снижению баллов по САТ-тесту: в группе 1 до 10 баллов, в группе 2 до 12 баллов (Z=2,013; p=0,044), в пользу комбинированного бронхолитика Тб/О. По другим показателям статистически значимого преимущества между группами не выявлено. На фоне приема комбинированного препарата ДДАХ/ДДБА пациенты группы 2 ТБ+ХОБЛ отмечали улучшение общего самочувствия, оцениваемое по такому совокупному показателю, как CAT-тест, который включает не только одышку, но и кашель, выделение мокроты, сон, повседневную активность, общее самочувствие, переносимость физических нагрузок.
Лечение ТБ осуществлялось в соответствии со стандартами терапии по I и III режимам терапии в зависимости от формы ТБ, наличия микобактерии туберкулеза (МБТ). В 1-й группе по I режиму терапию получали 17 (54,8%) пациентов, по III – 14 (45,2%) , во 2-й группе по I режиму – 18 (58,1%) пациентов, по III – 13 (41,9%).
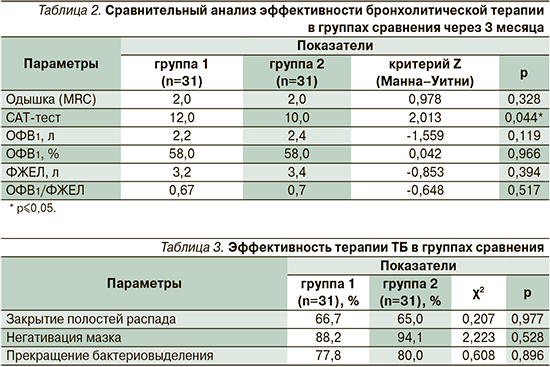
Эффективность терапии ТБ оценивалась по закрытию полостей распада, негативации мазка и прекращению бактериовыделения через 6 месяцев наблюдения (табл. 3).
Негативация мазка через 6 месяцев наблюдения была достигнута в 88,2% случаев в группе 1 (ДДАХ) и в 94,1% группе 2 (ДДАХ/ДДБА) соответственно (χ2=2,22; p=0,528), прекращение бактериовыделения – в 77,8 и 80,0% соответственно (χ2=0,608; p=0,896), закрытие полостей распада – в 66,7 и 65% соответственно (χ2=0,207; р=0,977).
Заключение
Включение в комплексную терапию пациентов с коморбидной патологией ТБ+ХОБЛ бронхолитиков длительного действия в качестве как монотерапии (ДДАХ), так и в комбинации (ДДАХ/ДДБА) сопровождается улучшением субъективной симптоматики спирометрических параметров. Применение бронхолитиков значительно уменьшает одышку, улучшает общее самочувствие, что косвенно способствует повышению приверженности лечению основного заболевания.
Купирование бронхообструктивного синдрома оказывает положительное влияние и на течение туберкулезного процесса. Восстановление вентиляции легочной ткани способствует лучшему отхождению мокроты, сокращению сроков абациллирования и закрытия полостей распада.
Использование комбинированного бронхолитика (ДДАХ/ДДБА) показало некоторые преимущества над монотерапией (ДДАХ) у пациентов с ТБ+ХОБЛ в отношении положительного совокупного влияния на состояние респираторной функции (САТ-тест).
Таким образом, использование в комплексной терапии комбинированного препарата ДДАХ/ДДБА длительного 24-часового действия тиотропия бромида/олодатерол (Спиолто Респимат) 2,5 мкг у пациентов ТБ+ХОБЛ позволяет уменьшать выраженность БОС, улучшать общее состояние пациентов, тем самым повышать приверженность лечению ТБ, что способствует сокращению сроков госпитализации, следовательно, затрат на стационарное лечение ТБ как наиболее экономически обременительного компонента терапии.